The Light Revolution: Redefining Vascular Health with Laser Technology
AUGUST 20, 2025
Phlebology, the medical specialty dedicated to the diagnosis and treatment of venous disorders, has undergone a transformative evolution over the past few decades. With the advent of minimally invasive techniques, particularly those involving advanced laser technology and sclerotherapy, the management of venous diseases such as varicose veins and spider veins has become significantly more effective, less painful, and marked by quicker recovery times. These innovations fall under the umbrella of Minimally Invasive Laser Medicine (MILM), a field that represents the forefront of high-tech medical care in phlebology, otolaryngology, and lymphology.
In this comprehensive guide, we will delve into the modern techniques in phlebology, focusing specifically on the comparative aspects of laser therapy and scleroth erapy. By examining their mechanisms, applications, advantages, disadvantages, and outcomes, this article aims to provide a thorough understanding of how these treatments contribute to the management of venous disorders.
Venous disorders represent a group of conditions that primarily affect the venous system, which plays a crucial role in transporting deoxygenated blood from various parts of the body back to the heart. Unlike arteries, veins rely on one-way valves and the contraction of surrounding muscles, particularly in the legs, to ensure efficient blood flow against gravity. When these valves weaken or become damaged, blood can pool within the veins, leading to increased venous pressure, dilation of the vessel walls, and a variety of clinical manifestations.
One of the most common venous disorders is varicose veins. These are enlarged, twisted, and bulging veins that typically appear on the legs due to prolonged standing or walking, which increases pressure in the lower extremities. While often dismissed as a cosmetic concern, varicose veins can cause symptoms such as aching, heaviness, fatigue, and swelling. In more advanced cases, they may contribute to skin changes, inflammation, and even ulcer formation if left untreated.
Another widespread condition is spider veins (telangiectasias). These are small, thin, red, purple, or blue veins that spread out in a web-like pattern on the surface of the skin. Though generally harmless, spider veins can be associated with discomfort, itching, or burning sensations. They often occur on the legs and face, and while they may not cause serious health problems, they frequently prompt patients to seek treatment for aesthetic reasons.
A more serious venous disorder is chronic venous insufficiency (CVI). This condition develops when the venous system fails to effectively return blood to the heart, resulting in persistent pooling of blood in the lower extremities. Symptoms include swelling of the legs and ankles, thickening or discoloration of the skin, eczema-like irritation, and, in advanced stages, venous ulcers that are difficult to heal. CVI not only affects quality of life but also increases the risk of complications such as infections or deep vein thrombosis (DVT).
In addition to these common disorders, venous disease may present in other forms such as phlebitis (inflammation of a vein, often associated with clot formation), deep vein thrombosis (potentially life-threatening clots in deep veins), and post-thrombotic syndrome, a chronic complication following DVT. Each of these conditions requires timely diagnosis and management to prevent progression and reduce health risks.
Understanding the pathophysiology of venous disorders is vital for selecting appropriate treatment strategies. The progression from mild spider veins to severe CVI reflects a continuum of venous dysfunction, and interventions must be tailored to the severity of the disease, patient health status, and long-term goals. Modern therapies, including minimally invasive laser medicine, compression therapy, sclerotherapy, and surgical techniques, provide a range of options to address both cosmetic and medical aspects of venous disease.
Minimally Invasive Laser Medicine (MILM) has revolutionized the field of phlebology by providing safe, efficient, and patient-friendly alternatives to traditional surgical methods such as vein stripping. Phlebology, the medical specialty dedicated to diagnosing and treating venous disorders, has long faced the challenge of offering treatments that are both effective and minimally disruptive. With the advent of advanced laser technologies, physicians can now deliver precise energy directly to diseased veins, sealing them shut and rerouting blood flow through healthier veins.
One of the primary advantages of MILM is its unparalleled precision. Unlike traditional methods that often require larger incisions and mechanical removal of the vein, laser energy can be directed with pinpoint accuracy, ensuring that only the problematic vein segment is treated. This minimizes damage to surrounding tissues, reduces postoperative pain, and lowers the risk of complications such as infection or nerve injury.
Another key benefit of MILM is its minimally invasive approach. Most procedures require only a small incision or a needle puncture for catheter insertion, significantly reducing trauma to the body. This means that patients often experience little to no scarring, faster healing, and fewer lifestyle interruptions compared to conventional surgery. For many individuals, this translates into same-day procedures performed on an outpatient basis, eliminating the need for lengthy hospital stays.
Recovery after MILM is remarkably quick. Most patients are encouraged to walk immediately after treatment, and many resume their normal daily activities within 24 hours. Light compression stockings are usually recommended for a short period post-procedure to support circulation and optimize healing. Compared to older surgical techniques that required weeks of recovery, MILM represents a significant improvement in patient convenience and quality of life.
In terms of clinical outcomes, MILM consistently demonstrates high success rates, with long-term vein closure exceeding 90–95% in many studies. Procedures like Endovenous Laser Therapy (EVLT) have become gold standards in modern phlebology due to their reliability and durability. Additionally, transdermal laser treatments are increasingly used for smaller surface veins, such as spider veins, providing excellent cosmetic results without the need for invasive surgery.
The combination of high efficacy, safety, and patient satisfaction has made MILM one of the most widely adopted approaches for venous disease worldwide. It has not only replaced many traditional surgical interventions but also expanded treatment accessibility to patients who previously avoided surgery due to fear of pain, downtime, or scarring.
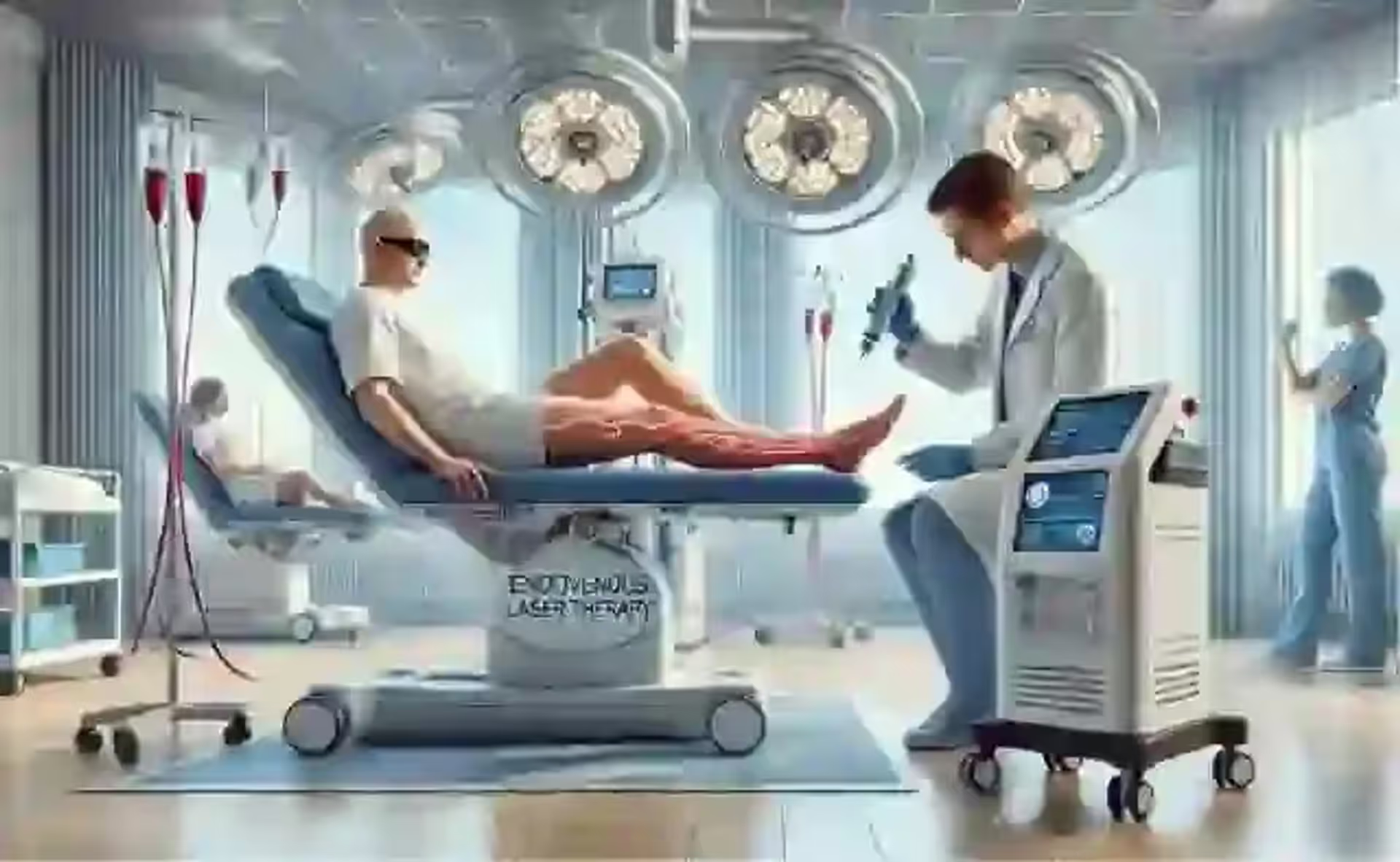
Laser therapy, and especially Endovenous Laser Therapy (EVLT), has become a cornerstone in the modern management of varicose veins. Unlike older, invasive surgical procedures such as vein stripping, laser therapy offers patients a minimally invasive, highly effective, and cosmetically superior treatment option. The use of targeted laser energy allows for precise closure of diseased veins while sparing surrounding healthy tissues, making it one of the safest and most efficient methods in contemporary phlebology.
How Laser Therapy Works. The procedure is performed under ultrasound guidance, ensuring that the affected veins are accurately mapped before treatment begins. Once the vein is located, the physician administers local anesthesia to the treatment area, significantly reducing discomfort during the procedure. A small puncture incision is made, through which a thin catheter is inserted into the vein. A specialized laser fiber is then threaded through the catheter until it reaches the diseased section of the vein.
When activated, the laser delivers controlled pulses of thermal energy to the vein wall. This energy causes the vein to collapse, contract, and eventually seal shut. Over time, the closed vein is reabsorbed by the body, and blood is naturally rerouted to healthier veins, restoring normal circulation. The entire process typically takes less than an hour and is performed in an outpatient setting, meaning patients can go home the same day.
Benefits of Laser Therapy. The advantages of EVLT over traditional methods are significant. As a minimally invasive procedure, it requires only a small puncture rather than large surgical incisions, which greatly reduces tissue trauma. Patients experience less pain and discomfort, both during and after treatment, compared to vein stripping or ligation. Recovery is remarkably fast—many patients are able to return to work and normal activities within 24–48 hours.
From a clinical perspective, EVLT boasts a long-term success rate exceeding 95%, making it one of the most reliable treatments for varicose veins. Its cosmetic benefits are also highly valued: since no major incisions are needed, scarring is minimal, and the overall appearance of the treated leg improves significantly once symptoms such as swelling and bulging veins resolve.
Potential Risks and Complications. While EVLT is generally safe, as with any medical procedure, there are potential risks. Bruising and swelling around the treated area are relatively common but typically resolve within a few days. In rare cases, temporary nerve irritation can occur, particularly when veins near sensory nerves are treated, though this usually improves with time. More serious complications such as deep vein thrombosis (DVT) or blood clots are extremely rare but require immediate medical attention. With proper technique and ultrasound monitoring, the risk of skin burns or thermal injury is very low.
Clinical Outlook. Laser therapy in phlebology continues to evolve with improvements in laser fiber design, wavelength technology, and energy delivery systems. These innovations are aimed at making the procedure even safer, more comfortable, and more effective. For most patients with varicose veins, EVLT represents the gold standard of care—offering a durable, minimally invasive solution that restores both vascular health and quality of life.
Sclerotherapy is a well-established, minimally invasive treatment designed to address both varicose veins and spider veins. It has been widely used for decades and remains one of the most common procedures in modern phlebology due to its simplicity, effectiveness, and cost-efficiency. The principle behind sclerotherapy lies in using a special solution, known as a sclerosant, to damage the inner lining of the targeted vein. This irritation causes the vein walls to stick together, eventually leading to closure of the vein. Over time, the body reabsorbs the treated vein, rerouting blood flow into healthier vessels.
How Sclerotherapy Works. The procedure is straightforward and usually performed in an outpatient clinic:
Sclerotherapy is not a one-size-fits-all treatment. Several variations exist to address different types and sizes of veins:
Liquid Sclerotherapy – The most traditional method, ideal for treating small spider veins and minor varicose veins near the skin’s surface.
Foam Sclerotherapy – Involves mixing the sclerosant with air or carbon dioxide to create a foam. This foam displaces blood inside the vein, allowing for better contact with the vein wall and making it more effective for larger or longer veins.
Ultrasound-Guided Sclerotherapy – Used for deeper or hidden veins that cannot be seen with the naked eye. Ultrasound imaging ensures that the sclerosant is injected precisely into the targeted vein, increasing both safety and efficacy.
Benefits of Sclerotherapy. The popularity of sclerotherapy is driven by several advantages:
Potential Risks and Complications
Although sclerotherapy is considered safe, some possible side effects and risks should be noted: Skin Discoloration – Temporary brown lines or spots may appear along the treated veins, usually resolving within a few months. Allergic Reactions – Rare, but possible with certain sclerosant agents. Pain or Cramping – Mild discomfort, burning, or cramping at the injection site is common but typically short-lived. Blood Clots (Thrombosis) – Rare but serious; larger treated veins may develop small clots, requiring additional treatment. Matting – In some cases, new small, fine blood vessels may appear near the treated area.
Sclerotherapy remains one of the most versatile and reliable treatments for venous disorders, particularly for patients with cosmetic concerns or smaller vein issues. It provides excellent results with minimal invasiveness, making it a preferred first-line treatment for spider veins and superficial varicose veins. For larger or deeper venous disease, sclerotherapy may be combined with other techniques such as endovenous laser therapy (EVLT) or radiofrequency ablation (RFA) to optimize outcomes.
When evaluating treatment options for venous disorders, laser therapy (most commonly Endovenous Laser Therapy, EVLT) and sclerotherapy are two of the most widely used and effective modalities. Both procedures are minimally invasive and designed to eliminate diseased veins, but they differ in terms of indications, methodology, and long-term outcomes. Choosing the most appropriate treatment depends on the patient’s vein condition, overall health, and personal preferences, as well as the expertise of the treating physician.
Effectiveness. Laser therapy has proven to be highly effective for treating larger, deeper varicose veins, with success rates exceeding 95% in clinical studies. Its durability makes it the preferred choice for patients seeking long-term relief from significant venous insufficiency. The heat energy from the laser not only closes the diseased vein but also reduces the risk of recurrence.
Sclerotherapy, on the other hand, involves injecting a chemical solution (sclerosant) directly into the vein, causing it to collapse and eventually fade. It is considered the gold standard for small to medium-sized veins, such as spider veins and reticular veins, but its effectiveness decreases when treating larger varicose veins. In such cases, multiple treatment sessions may be required, and recurrence rates tend to be higher compared to EVLT.
Procedure Time. Both procedures are relatively quick, performed on an outpatient basis. Laser therapy typically takes 30 to 60 minutes, depending on the number and length of veins being treated. Sclerotherapy sessions are shorter, often lasting less than 30 minutes, especially when treating small surface veins. However, since sclerotherapy may require multiple sessions to achieve optimal results, the overall time investment for the patient can sometimes be greater than with EVLT.
Recovery Time. Laser therapy usually involves a brief recovery period, with most patients able to resume normal activities within 24 to 48 hours. Some mild bruising or tightness along the treated vein may occur but generally resolves quickly.
Sclerotherapy offers an almost immediate return to normal activities, making it very convenient. However, patients are usually advised to wear compression stockings for several days to promote healing and maximize treatment effectiveness. For cosmetic spider vein treatments, noticeable improvements may take several weeks, as the veins gradually fade from view.
Pain and Discomfort. With laser therapy, patients may experience mild discomfort or heat sensations during the procedure, but this is well-managed with local anesthesia. Post-procedural soreness is minimal and short-lived.
Sclerotherapy typically causes a slight burning, tingling, or cramping sensation at the injection site. These sensations are usually brief, though some patients may notice localized redness or itching afterward.
Cost. Laser therapy generally involves a higher upfront cost due to the advanced equipment and technology required. However, its high long-term success rate often makes it cost-effective in the long run, especially for patients with significant venous disease.
Sclerotherapy is less expensive per session, making it attractive for cosmetic purposes and smaller vein treatments. Yet, since multiple sessions are often necessary, the overall cost may accumulate over time, particularly when treating larger or more complex venous conditions.
Cosmetic Outcomes. Laser therapy provides excellent results for large varicose veins, with minimal scarring and significant improvement in both function and appearance. The treated veins collapse and gradually disappear, leaving smoother and healthier-looking skin.
Sclerotherapy remains the preferred method for purely cosmetic treatments, especially for spider veins and small varicose veins, where precision and minimal invasiveness are key. It delivers high patient satisfaction in terms of aesthetics, but its effectiveness for larger veins is limited compared to EVLT.
In modern phlebology, many patients present with a combination of venous disorders, ranging from large, dilated varicose veins to fine spider veins visible on the skin’s surface. Treating these conditions with a single technique often provides incomplete results. This is where the integration of laser therapy (such as Endovenous Laser Therapy, EVLT) and sclerotherapy proves especially valuable, as it enables physicians to address the entire spectrum of venous disease in a more comprehensive manner.
Laser therapy is highly effective in closing larger veins, such as the saphenous vein, which often acts as the underlying source of venous reflux. Once the refluxing trunk vein is sealed with laser energy, smaller branches and superficial spider veins can then be treated with sclerotherapy. This stepwise, layered approach ensures that the root cause of venous insufficiency is corrected, while also improving the cosmetic appearance of the legs.
Combination Therapy Benefits:
Clinical Practice Applications: In practice, many physicians begin with EVLT or another form of endovenous ablation to treat large varicose veins. Following healing, sclerotherapy sessions are scheduled to remove residual smaller veins and spider veins, ensuring a smooth aesthetic result. This staged, integrative strategy has become a gold standard in advanced vein clinics worldwide. Moreover, integrating both therapies often reduces the need for invasive surgery, shortens recovery times, and provides patients with a more complete sense of resolution—both in terms of symptoms and appearance. For patients, this translates into greater satisfaction and long-lasting improvements in vascular health.
Post-Treatment Care and Long-Term Management. Successful treatment of varicose veins and other venous disorders does not end in the operating room or clinic—it continues with proper post-treatment care and thoughtful long-term management. Regardless of whether the chosen therapy was endovenous laser therapy (EVLT), sclerotherapy, or another minimally invasive approach, the patient’s recovery and long-term results largely depend on adherence to medical recommendations and lifestyle adjustments.
Key Post-Treatment Recommendations
Compression Stockings. Wearing compression stockings is one of the most important steps after treatment. These specially designed garments apply graduated pressure to the legs, helping to reduce swelling, prevent blood from pooling, and support proper venous circulation. The duration of use depends on the treatment performed and the severity of the condition, but most patients are advised to wear them daily for at least 1–2 weeks post-procedure.
Physical Activity. Light physical activity, particularly walking, is highly encouraged after treatment. Walking activates the calf muscles, which function as a natural pump to push blood back toward the heart. Patients are typically advised to walk for at least 10–20 minutes several times a day and gradually increase activity levels while avoiding strenuous exercise during the initial recovery phase.
Avoiding Prolonged Standing or Sitting. Extended periods of immobility increase venous pressure and the risk of recurrence. Patients are encouraged to take regular breaks to stretch, walk, or shift positions, especially if they work in occupations that involve long hours of sitting or standing. Elevating the legs when resting can also improve circulation and reduce discomfort.
Follow-Up Visits. Regular follow-up appointments are essential to evaluate treatment success, monitor for complications, and detect early signs of recurrence. Ultrasound examinations may be performed to ensure that treated veins remain closed and that blood flow is properly rerouted. Follow-ups also provide an opportunity for patients to discuss symptoms, cosmetic results, and preventive strategies with their physician.
Long-term management is focused on maintaining vascular health and preventing the recurrence of venous disorders. This requires a combination of healthy lifestyle practices and risk factor control:
Post-treatment care and long-term management are as important as the initial therapy itself. By following medical guidance, adopting an active lifestyle, and addressing risk factors, patients can significantly reduce the risk of recurrence and enjoy lasting improvements in both health and quality of life. With ongoing care and preventive strategies, modern treatments like EVLT and sclerotherapy can provide not only cosmetic benefits but also long-term relief from the discomfort and complications associated with venous disorders.
Modern techniques in phlebology, particularly laser therapy and sclerotherapy, have fundamentally transformed the management of venous disorders. Where traditional surgical interventions often required extended hospital stays, significant recovery times, and carried higher risks of complications, today’s minimally invasive approaches have set a new benchmark for both safety and effectiveness. Minimally Invasive Laser Medicine (MILM), in particular, has redefined standards of patient care, offering procedures that are not only clinically successful but also minimally traumatic, cosmetically superior, and convenient for patients.
Both laser therapy and sclerotherapy hold distinct strengths, and their application depends largely on the size, depth, and severity of the diseased veins. Laser therapy is especially effective for larger varicose veins, delivering precise energy to seal affected vessels, while sclerotherapy excels in treating smaller varicosities and spider veins. In many cases, these two techniques complement each other, allowing physicians to develop tailored treatment strategies that address both functional and aesthetic concerns. This patient-centered approach ensures that therapy is not only about eliminating symptoms but also about restoring confidence, mobility, and quality of life.
Equally important is the role of patient education and long-term management. Understanding the mechanisms, benefits, and limitations of each treatment empowers patients to make informed decisions in collaboration with their healthcare providers. Moreover, adopting preventive lifestyle changes—such as maintaining an active routine, managing weight, and wearing compression stockings when necessary—can significantly enhance long-term outcomes and reduce recurrence rates.
Looking ahead, the future of phlebology is bright, with continuous advancements in laser technologies, imaging systems, robotics, and artificial intelligence. These innovations promise to make treatments even more precise, efficient, and accessible, reducing procedure times and further minimizing risks. Additionally, the integration of personalized medicine, where therapies are adapted to the unique vascular anatomy and genetic profile of each patient, holds the potential to revolutionize outcomes in venous care.
In conclusion, phlebology has entered a new era in which minimally invasive, patient-friendly therapies are the gold standard. By combining cutting-edge technology with comprehensive patient care, modern medicine is not only treating venous disorders more effectively than ever before but also enhancing the overall well-being of patients worldwide.